3 Food-Based Supplements for Your Gut Microbiome
Posted by admin on
Nutrient sufficiency is arguably the most important quality of any dietary approach, meaning we choose whole foods with the goal of consuming adequate quantities of all essential and nonessential nutrients required by biological processes in our bodies (see The Importance of Nutrient Density, my book Paleo Principles and my online course Therapeutic Paleo Approach). Emerging evidence shows that our gut bacteria, too, require certain nutrients—and that these are essential for their growth, health, and metabolism. Our gut bacteria must necessarily obtain these nutrients from the food that we eat, and as is the case with the rest of our bodies, the state of our gut microbiome is impacted when we consume either too little or extreme excess of these nutrients. See also What Is the Gut Microbiome? And Why Should We Care About It?
Yes, we can add yet another reason to eat organ meat and shellfish to the list: A nutrient-dense diet supports a healthy gut microbiome! But, I recognize that some of the most important superfoods that we can eat are, how shall I put this, er, not so tasty? Lol! So, instead of yet another article highlighting the value of liver and oysters (see for example Why Everyone Should Be Eating Organ Meat and Oysters, Clams, and Mussels, Oh My! Nutrition Powerhouses or Toxic Danger? ), let’s keep it simple and focus on three food-based supplements to support the microbiome (and us!)!
Organic 3 Beef Liver Capsules for Vitamin A (and more!)
 In addition to containing impressive amounts of dozens of important vitamins and minerals, liver is one of the most concentrated sources of vitamin A of any food, and is an outstanding source of vitamin D, vitamin B12 (and other B vitamins), copper, potassium, magnesium, phosphorous, manganese, and iron in the heme form that is readily absorbed and used by the body. And it just so happens that every single one of these nutrients is essential to support a healthy and diverse gut microbiome.
In addition to containing impressive amounts of dozens of important vitamins and minerals, liver is one of the most concentrated sources of vitamin A of any food, and is an outstanding source of vitamin D, vitamin B12 (and other B vitamins), copper, potassium, magnesium, phosphorous, manganese, and iron in the heme form that is readily absorbed and used by the body. And it just so happens that every single one of these nutrients is essential to support a healthy and diverse gut microbiome.
Vitamin A for the Gut Microbiome
Not to be confused with beta-carotene (which is a vitamin A precursor, not vitamin A itself), vitamin A (retinol) is essential for bone growth, tooth remineralization, skin health, vision, reproduction, and immune function. It also is essential for gut barrier health in addition to its specific impact on the composition of the gut microbiome.
In children with persistent diarrhea, those with measured vitamin A deficiency had significantly lower bacterial diversity (diversity is a hallmark feature of a healthy gut microbiome), a higher proportion of problematic Enterococcus species, and a reduction in important butyrate-producing bacteria compared to children with normal vitamin A levels.
In rats, vitamin A deficiency has also been shown to increase the total amount of bacteria in the GI tract (implying vitamin A deficiency can contribute to bacterial overgrowth, for example SIBO), suppress levels of Lactobacillus species, and lead to the appearance of pathogenic Escherichia coli strains. In a mouse model of autoimmune lupus, vitamin A supplementation restored levels of Lactobacillus that were depleted in the lupus-prone mice, correlating with improved symptoms.
In one study of mice inoculated with a murine version of norovirus (the most frequent viral cause of acute gastroenteritis worldwide), administration of retinoic acid (a vitamin A metabolite) inhibited the replication of norovirus, as well as favorably shifted the composition of the gut microbiota. More specifically, retinoic acid treatment significantly increased the abundance of Bifidobacterium, Aggregatibacter, Allobaculum, Dialister, and Enhydrobacter, and increased the abundance of Lactobacillus that was suppressed by norovirus administration. The increase in Lactobacillus appeared to be responsible for the inhibitory effects of retinoic acid against norovirus. In a later study, the same researchers further investigated the mechanisms behind vitamin A’s antiviral activity and found that Lactobacillus species significantly increased the expression the cytokines interferon-β (IFN-β) and IFN-γ, indicating that the activation of interferons by vitamin A via an increase in Lactobacillus plays a critical role in the body’s immune response against norovirus.
Another study of vitamin A deficient versus vitamin A sufficient mice found that the deficient animals had lower levels of butyrate, Clostridium_XVIII, Roseburia, Pseudomonas, Blautia, Parabacteroides, Pseudomonadaceae, Bacteroidia, and Bacteroidetes and higher levels of acetate, Johnsonella, and Staphylococcaceae; the Firmicutes/Bacteroidetes ratio was also higher (linked to obesity and diabetes). In addition, vitamin A significantly affected bacterial pathways involved in macronutrient metabolism: the bacterial pathways in the deficient mice had enhanced amino acid and carbohydrate metabolism associated with lower amino acid biosynthesis, indicating that vitamin A deficiency interferes with the microbiota’s ability to produce and metabolize these nutrients.
Freeze-dried Beef Liver Capsules by Organic 3
Liver stands out as a gut microbiome superfood because of its overall high density of essential nutrients as well as being such a valuable source of vitamin A. And, the most convenient way to add quality liver to our daily diet is with Organic 3 Beef Liver Capsules.
Organic 3 sources grass-fed beef liver from New Zealand for its Beef Liver Capsules. The liver is non-defatted to preserve its fat-soluble nutrient content (including vitamin A) and it’s freeze-dried, which also helps preserve the full range of nutrients compared to desiccated liver capsules thanks to maintaining cold temperatures through the drying process. There’s no additives or fillers and the capsules are simply made from gelatin.
Organic 3 Beef Liver Capsules are available online from Corganic. I love Corganic and truly appreciate the care and precision that Corganic puts into curating their online store containing only top-quality nourishing foods and innovative supplements designed to maximize our benefit from a nutrient-dense anti-inflammatory diet. Their philosophy is completely aligned with my own!
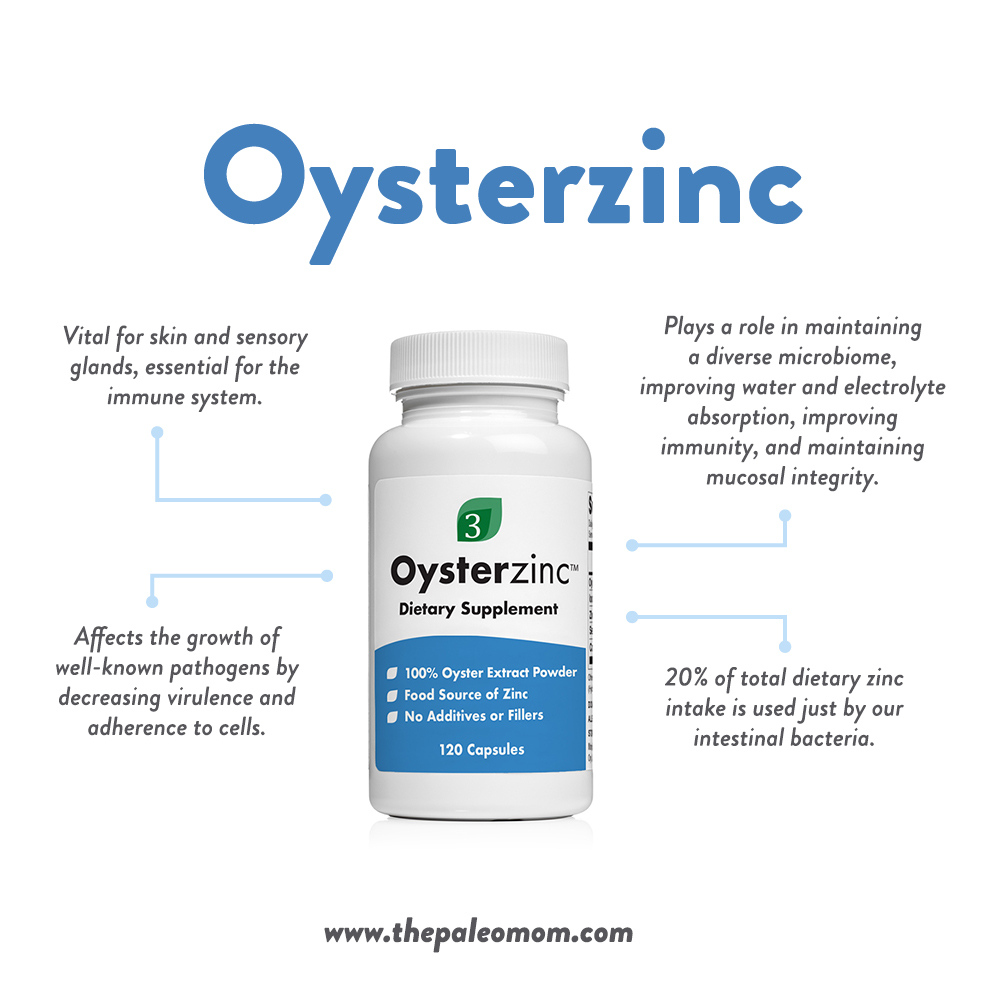
Organic 3 Oysterszinc™ for Zinc and Selenium
 Oysters are the richest food source of zinc, but are also amazing sources of vitamin D, vitamin B12, selenium, copper, and iron, and contain good amounts of vitamins B1, B2, B3, C, (yes, vitamin C), calcium, magnesium, manganese, phosphorus, and potassium, and oysters even provide some vitamins A, B5, B6, B9 and E plus dozens of trace minerals. In fact, oysters rival liver in terms of nutrient-density, while complementing the nutrients in liver well.
Oysters are the richest food source of zinc, but are also amazing sources of vitamin D, vitamin B12, selenium, copper, and iron, and contain good amounts of vitamins B1, B2, B3, C, (yes, vitamin C), calcium, magnesium, manganese, phosphorus, and potassium, and oysters even provide some vitamins A, B5, B6, B9 and E plus dozens of trace minerals. In fact, oysters rival liver in terms of nutrient-density, while complementing the nutrients in liver well.
Let’s zoom in on zinc and selenium in particular, since these two minerals are essential for the gut microbiome and since oysters are particularly impressive sources of them.
Zinc for the Gut Microbiome
Important for nearly every cellular function, from protein and carbohydrate metabolism to cell division and growth. Zinc also plays a role in skin health and the maintenance of sensory organs (that’s why zinc deficiency is associated with a loss of smell and taste) and is a vital nutrient for immune system function. Zinc also plays a vital role in epithelial barrier function by improving tight junction formation. The richest source is oysters, but other good sources include red meat, poultry, nuts and seeds, and legumes.
The gut microbiota has a two-way relationship with the mineral zinc: not only does zinc availability influence the composition of the microbiota, but the microbiota composition also influences the levels of zinc within the body!
Specifically, dietary zinc deficiency has been shown to decrease overall species diversity and richness in the gut microbiota (that’s a bad thing!), leading to reduced production of short-chain fatty acids (also bad!). Furthermore, the zinc-deficiency-induced alterations in microbiota could subsequently limit the absorption and availability of ingested zinc, leading to a negative feedback cycle that could worsen existing zinc deficiency. In fact, as early as the 1970s, research on the gut microbiota showed that conventionally raised mice had dietary zinc requirements that were nearly double that of germ-free mice (microbially sterile mice used for microbiome research), confirming a role of gut microbes in zinc homeostasis. Actually, about 20% of our dietary zinc intake is used just by our intestinal bacteria. More recently, researchers discovered that some bacterial species, including the diarrheal pathogen Campylobacter jejuni, compete for zinc within the intestine, and that zinc deficiency could therefore preferentially spur the growth of bacteria that thrive in low-zinc conditions.
Researchers compared the impact on the microbiome (in mice) of a diet low in total zinc versus a diet containing adequate zinc but also zinc uptake inhibitors (including phytic acid!) to decrease the bioavailability of the zinc versus a control diet with adequate zinc. Both the zinc-deficient and zinc-inhibited diets caused major disruptions to the microbiome, but some species thrived under zinc-inhibited conditions (including Actinobacteria, Lachnospiraceae, and Bacteriodetes species) that did not grow under zinc-deficient conditions, indicating that some bacteria are able to successfully compete for zinc in the presence of zinc uptake inhibitors. And while many important probiotic species were reduced in both the zinc-deficient and zinc-inhibited diets, other bacteria (in particular, the family Lachnospiraceae) were able to thrive in low-zinc conditions. Importantly, these bacterial shifts coincided with changes in markers of gut barrier health as well as significantly higher levels of E. coli endotoxin in the liver, indicating increased intestinal permeability. What’s more, those changes in gut physiology had consequences for the brain: both the zinc-deficient and zinc-inhibited diets resulted in elevated levels of the inflammatory cytokines interleukin-6 and interleukin-1β in the brain, indicating neuroinflammation.
The takeaway from this important experiment? Not only is ingesting adequate zinc imperative for maintaining a healthy gut (and brain!), but so is ingesting enough bioavailable zinc. Although some bacteria have mechanisms that allow them to compete with zinc uptake inhibitors, many don’t. Therefore, zinc-rich plant foods that are also high in phytate (such as nuts, legumes, and grains) may not be the best place to get our zinc needs met. Oysters to the rescue!
Zinc also decreases the growth of well-known pathogens. For example, zinc decreases the virulence and adherence to cells of enteropathogenic E. coli—a strain of E. coli that adheres to intestinal cells and is responsible for watery diarrhea. In one study of fecal microbiota transplant recipients, after adjusting for potential confounders, zinc deficiency was associated with an increased risk of recurrence of C. difficile infection, and zinc supplementation among those who were deficient reduced this risk—potentially due to zinc’s role in maintaining a diverse microbiome, improving water and electrolyte absorption, improving immunity, and maintaining mucosal integrity.
There’s also a really good argument for getting zinc from whole food sources. In a study of mice colonized with C. difficile, excess zinc supplementation (12 times the level found in adequate zinc control diet) changed the microbiota in a way that resembled antibiotic treatment, increased toxin activity, lowered the amount of antibiotics needed to induce susceptibility to infection, and dramatically worsened how severe and lethal the C. difficile-associated disease was. The mechanism involved the zinc-binding protein calprotectin, which exerts antimicrobial effects against C. difficile by limiting the amount of zinc (which is needed by C. difficile) within the intestinal track. Excess dietary zinc, in turn, prevented calprotectin from adequately interfering with the metal uptake of C. difficile and allowed infection to progress. Given zinc’s popularity as an immune-boosting supplement, these findings highlight a potential danger of pushing intake too far beyond what’s provided in a nutrient-dense, whole foods diet. Oysters to the rescue again!
Selenium for the Gut Microbiome
Selenium is required for the activity of twenty-five to thirty different enzymes that protect the human brain and other tissues from oxidative damage. Selenium also helps support normal thyroid function. Good sources include oysters and other shellfish, red meat, poultry, fish, Brazil nuts, and mushrooms.
Because selenium is utilized by some microorganisms and is toxic to others, dietary selenium can influence the composition of the microbiota. About 25% of all bacteria express selenoproteins (and therefore require selenium to grow optimally), and these bacteria increase the selenium requirement of their host due to using it for their own growth.
In a study of mice placed on diets that were deficient, adequate, or enriched in selenium, gut microbial diversity increased as selenium intake increased (high diversity is one of the most important hallmarks of a healthy microbiome). In chickens, selenium increased the abundance of probiotics Lactobacillus and Faecalibacterium, as well as increased gut levels of short-chain fatty acids (particularly butyric acid). On the flip side, selenium deficiency alters the gut microbiota composition in ways that increases susceptibility to Salmonella typhimurium infection and chemically induced colitis.
In a variety of studies, supplementing with selenium-enriched probiotics shows synergistic effects beyond either probiotic bacteria alone or selenium alone. For example, in mice, selenium-enriched probiotics (Candida utilis, Lactobacillus acidophilus, Lactobacilus rhamosus GG, and Streptococcus thermophilus) were better able to inhibit E. coli infection and mortality than probiotics or selenium alone. In piglets, animals fed selenium-enriched probiotics (in this case, Lactobacillus acidophilus and Saccharaomyces verevisiae) saw greater increases in blood selenium levels than the selenium-only or probiotic-only groups, and also suppressed E. coli levels and reduced incidence of diarrhea, suggesting the combination of probiotics and selenium can benefit the gut ecosystem as well as selenium homeostasis.
Organic 3 Oysterzinc™
Oysters stand out as a gut microbiome superfood because of their overall high density of essential nutrients as well as being such a valuable source of zinc and selenium. And, the most convenient way to add quality oysters to our daily diet is with Organic 3 Oysterzinc™.
Organic 3 sources oysters from the pristine Atlantic waters along Ireland’s lush coastline, dehydrated by a proprietary artisan process. Oysterzinc™ is 100% pure oyster powder, made from only the extracted meat of the oyster with no shell included, as well as no additives or fillers. Each bottle contains the extracted goodness of over 60 oysters!
Organic 3 Oysterzinc™ is also available from Corganic. (Full disclosure: the capsules smell terrible! You’ll want to swallow them quickly and hold your breath for that second in between putting them in your mouth and raising your glass of water to your mouth to wash them down!)
Rosita Extra Virgin Cod Liver Oil for Vitamin D and Omega-3 Fats
 Rosita Extra Virgin Cod Liver Oil is the only fresh, sustainably- and wild-caught and raw cod liver oil on the market. It contains naturally-occurring vitamins A and D, and a full spectrum of omega fatty acids, including the super important long-chain omega-3 fatty acids EPA and DHA. And these nutrients are very beneficial for the gut microbiome!
Rosita Extra Virgin Cod Liver Oil is the only fresh, sustainably- and wild-caught and raw cod liver oil on the market. It contains naturally-occurring vitamins A and D, and a full spectrum of omega fatty acids, including the super important long-chain omega-3 fatty acids EPA and DHA. And these nutrients are very beneficial for the gut microbiome!
Vitamin D for the Gut Microbiome
Assists in calcium absorption, immune system function, bone development, modulation of cell growth, neuromuscular function, and the reduction of inflammation. Although vitamin D can be produced when the sun’s UV rays hit the skin and trigger vitamin D synthesis, it also can be obtained from foods, including oily fish (such as salmon, tuna, and mackerel), mushrooms, fish roe, liver, and eggs.
Vitamin D routinely makes headlines for its importance in both physical and mental health, and it turns out, the gut microbiome is a major mediator for the benefits we credit to vitamin D!
The link between vitamin D and the gut microbiome may actually be a two-way street. While vitamin D can impact the health and composition of the gut, certain bacteria in the gut may also influence vitamin D levels in the blood by influencing vitamin D metabolism. In humans, higher levels of Coprococcus and Bifidobacterium, for instance, appear to promote higher vitamin D levels, though more studies are needed to definitely establish causality.
Vitamin D deficiency is linked with gut dysbiosis and inflammation, including severe colitis. Additional research shows vitamin D deficiency may contribute to metabolic syndrome (that nasty combination of obesity, insulin resistance, and cardiovascular disease risk factors) by aggravating diet-induced imbalances in the microbiota, including by decreasing the production of defensins (anti-microbial molecules needed for maintaining healthy gut flora). In rodents, vitamin D supplementation appears to improve metabolic syndrome via effects on the gut microbiome. And, people with higher levels of vitamin D have been shown to have lower levels of harmful endotoxin in the blood, possibly due to vitamin D’s ability to improve gut barrier integrity as well as normalizing the gut microbiome.
In human studies, vitamin D supplementation alters the composition of the gut microbiome, significantly reducing levels of Gammaproteobacteria (including the most common opportunistic pathogens Pseudomonas and Escherichia/Shigella), and increasing bacterial diversity (again, one of the signature features of a healthy microbiome!). Vitamin D also promotes the growth of beneficial species of Bacteroiodes and Parabacteroides (like species of Ruminococcaceae and Lachnospira), while inhibiting the growth of problematic species like Blautia.
With vitamin D, as with all nutrients, it’s possible to get much of a good thing. In a mouse model of colitis, animals were supplemented with high-dose vitamin D (10,000 IU/kg), moderate vitamin D (2280 IU/kg), or no vitamin D. The mice receiving the highest dose developed the most severe colitis, and the high-dose control group (receiving vitamin D but not exposed to dextran sodium sulphate to induce colitis) ended up with microbiota compositions that were similar to those of the DSS-treated group, including a rise in Sutterella—suggesting that the high vitamin D dosing caused a shift to a pro-inflammatory microbiome. Additionally, the high-dose vitamin D mice saw a significant drop in serum vitamin D levels in conjunction with developing colitis, likely due to vitamin D metabolites dropping in response to intestinal inflammation that was caused by excessive vitamin D intake. In humans, similar undesirable shifts in the microbiome are seen when serum vitamin D levels are in excess of 75ng/mL. This is yet another reason to test-not-guess when it comes to high-dose vitamin D supplementation, and highlights the importance of repeated testing (ideally every 3 months) when taking vitamin D3 supplements (to dial in your individual dose to achieve the ideal serum vitamin D levels between 50 and 70ng/mL). In the absence of repeated testing, natural (not high-dose) ways to improve vitamin D levels include plenty of sun exposure and food sources of vitamin D, like Rosita Extra Virgin Cod Liver Oil.
Omega 3 Fats for the Gut Microbiome
In case we need another reason to embrace seafood, here it is: omega-3 fats are among the most gut-friendly fats around! In fact, many of the benefits attributed to omega-3 fats on human health are mediated by the gut microbiome. Fish and shellfish are the richest food sources of the two long-chain omega-3 fatty acids, docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA). DHA is abundant in the brain and retinas and plays a role in maintaining normal brain function, treating mood disorders, and reducing risk of heart disease (or improving outcomes for people who already have it). The richest sources are fatty fish, such as salmon, mackerel, tuna, herring, and sardines. EPA plays a role in anti-inflammatory processes and the health of cell membranes and may help reduce symptoms of depression. Sources include fatty fish and algae.
Animal studies have helped elucidate the omega-3, gut, and disease connection. In mice, analyses of gut microbes and fecal transfers have shown that higher levels of omega-3 fats in body tissue are associated with greater production and secretion of intestinal alkaline phosphatase (an enzyme that splits cholesterol and long chain fatty acids). This leads to changes in the composition of gut bacteria that ultimately reduce endotoxin production, gut permeability, metabolic endotoxemia, and inflammation, all of which influence disease risk. Additional studies in mice have shown that omega-3-rich diets increase populations of important Lactobacillus and Bifidobacteria bacteria.
In humans, omega-3 supplementation leads to lower levels of Faecalibacterium and greater levels of butyrate-producing bacteria (particularly from the genera Eubacterium, Roseburia, Anaerostipes, and Coprococcus), along with higher levels of the essential probiotics Bifidobacterium and Lactobacillus. Likewise, higher omega-3 levels (reflecting higher consumption) have been linked to more microbial diversity in the gut, as well as a greater abundance of short-chain fatty acid-producing bacteria belonging to the Lachnospiraceae family. Omega-3 fats also appear capable of reversing the dysbiosis associated with irritable bowel disease, and their anti-inflammatory effects can benefit other disorders involving inflammation of the gut.
Omega-3 intake during pregnancy could even influence the offspring’s risk of obesity through gut-mediated mechanisms. One study using fat-1 transgenic mice (which produce high levels of endogenous omega-3 fats) and wild-type mice found that a lower ratio of omega-3 to omega-6 fatty acids in a mother’s body during pregnancy and breastfeeding altered the balance of gut microflora in her offspring, induced indicators of metabolic disruption, and led to significantly more weight gain. Another study using fat-1 mice found that higher levels of tissue omega-3 helped prevent gut dysbiosis induced by early exposure to antibiotics and protected against obesity, insulin resistance, fatty liver, and dyslipidemia later in life.
Rosita Extra Virgin Cod Liver Oil
Rosita Extra Virgin Cod Liver Oil is a very unique and quality source of vitamins A and D as well as DHA and EPA. Authentic cod (Gadus morhua) are sustainably caught, hook and line, on family fishing boats in the clean, crystal-clear Norwegian Hegland fjords. Rosita gently extracts their extra virgin cod liver oil using a patented technique that naturally releases the oil from the hand-picked livers without heat, chemicals, solvents or mechanics, which ensures the truly raw oil that is unadulterated, pure and safe with all of its rich nutrients intact. This is important because one of the problems with a lot of fish oils is that processing under heat causes oxidation of the fats. While a tiny drop of rosemary herb and full-spectrum vitamin E (from sunflower seeds) is added to maintain freshness, nothing is added to mask its clean all-natural taste of fresh fish. (It’s also available in a fish collagen capsule if you prefer.) Each batch is 3rd-party tested in a microbiological laboratory and certified to meet strict European regulations for potency and purity.
While eating plenty of vegetables and fruit is essential for a healthy and diverse gut microbiome (see also What Is the Gut Microbiome? And Why Should We Care About It?, Why Root Veggies Are Great for the Gut Microbiome, 5 Reasons to Eat More Fiber, and The Importance of Vegetables), our fiber consumption is just the tip of the iceberg in terms of how our food choices impact the composition and health of our gut microbiome, which in turn are determinants of our health. Our gut microbes are also sensitive to the amount and quality of the proteins we consume, the fats we consume, phytochemicals and the overall nutrient density of our diets. Yet another check in the “pro” column for a nutrient-focused diet, and obtaining the vital nutrients that both we and our gut microbiomes need from quality food sources!
Citations
Amit-Romach E, Uni Z, Cheled S, Berkovich Z, Reifen R. Bacterial population and innate immunity-related genes in rat gastrointestinal tract are altered by vitamin A-deficient diet. J Nutr Biochem. 2009 Jan;20(1):70-7. doi: 10.1016/j.jnutbio.2008.01.002.
Bashir M, Prietl B, Tauschmann M, Mautner SI, Kump PK, Treiber G, Wurm P, Gorkiewicz G, Högenauer C, Pieber TR. Effects of high doses of vitamin D3 on mucosa-associated gut microbiome vary between regions of the human gastrointestinal tract. Eur J Nutr. 2016 Jun;55(4):1479-89. doi: 10.1007/s00394-015-0966-2.
Bunnell BE, Escobar JF, Bair KL, Sutton MD, Crane JK. Zinc blocks SOS-induced antibiotic resistance via inhibition of RecA in Escherichia coli. PLoS One. 2017 May 22;12(5):e0178303. doi: 10.1371/journal.pone.0178303
Charoenngam N, Shirvani A, Kalajian TA, Song A, Holick MF. The Effect of Various Doses of Oral Vitamin D3 Supplementation on Gut Microbiota in Healthy Adults: A Randomized, Double-blinded, Dose-response Study. Anticancer Res. 2020 Jan;40(1):551-556. doi: 10.21873/anticanres.13984.
Crane JK, Naeher TM, Shulgina I, Zhu C, Boedeker EC. Effect of zinc in enteropathogenic Escherichia coli infection. Infect Immun. 2007 Dec;75(12):5974-84.
Gangadoo S, Bauer BW, Bajagai YS, Van TTH, Moore RJ, Stanley D. In vitro growth of gut microbiota with selenium nanoparticles. Anim Nutr. 2019 Dec;5(4):424-431. doi: 10.1016/j.aninu.2019.06.004.
Gangadoo S, Dinev I, Chapman J, Hughes RJ, Van TTH, Moore RJ, Stanley D. Selenium nanoparticles in poultry feed modify gut microbiota and increase abundance of Faecalibacterium prausnitzii. Appl Microbiol Biotechnol. 2018 Feb;102(3):1455-1466. doi: 10.1007/s00253-017-8688-4
Ghaly S, Kaakoush NO, Lloyd F, McGonigle T, Mok D, Baird A, Klopcic B, Gordon L, Gorman S, Forest C, Bouillon R, Lawrance IC, Hart PH. High Dose Vitamin D supplementation alters faecal microbiome and predisposes mice to more severe colitis. Sci Rep. 2018 Jul 31;8(1):11511. doi: 10.1038/s41598-018-29759-y.
Hibberd MC, Wu M, Rodionov DA, Li X, Cheng J, Griffin NW, Barratt MJ, Giannone RJ, Hettich RL, Osterman AL, Gordon JI. The effects of micronutrient deficiencies on bacterial species from the human gut microbiota. Sci Transl Med. 2017 May 17;9(390). pii: eaal4069. doi: 10.1126/scitranslmed.aal4069.
Kasaikina MV, Kravtsova MA, Lee BC, Seravalli J, Peterson DA, Walter J, Legge R, Benson AK, Hatfield DL, Gladyshev VN. Dietary selenium affects host selenoproteome expression by influencing the gut microbiota. FASEB J. 2011 Jul;25(7):2492-9. doi: 10.1096/fj.11-181990.
Lee H, Ko G. Antiviral effect of vitamin A on norovirus infection via modulation of the gut microbiome. Sci Rep. 2016 May 16;6:25835. doi: 10.1038/srep25835.
Lee H, Ko G. New perspectives regarding the antiviral effect of vitamin A on norovirus using modulation of gut microbiota. Gut Microbes. 2017 Nov 2;8(6):616-620. doi: 10.1080/19490976.2017.1353842.
Lv CH, Wang T, Regmi N, Chen X, Huang K, Liao SF. Effects of dietary supplementation of selenium-enriched probiotics on production performance and intestinal microbiota of weanling piglets raised under high ambient temperature. J Anim Physiol Anim Nutr (Berl). 2015 Dec;99(6):1161-71. doi: 10.1111/jpn.12326.
Lv Z, Wang Y, Yang T, Zhan X, Li Z, Hu H, Li T, Chen J. Vitamin A deficiency impacts the structural segregation of gut microbiota in children with persistent diarrhea. J Clin Biochem Nutr. 2016 Sep;59(2):113-121.
Naderpoor N, Mousa A, Fernanda Gomez Arango L, Barrett HL, Dekker Nitert M, de Courten B. Effect of Vitamin D Supplementation on Faecal Microbiota: A Randomised Clinical Trial. Nutrients. 2019 Nov 27;11(12). pii: E2888. doi: 10.3390/nu11122888.
Niccum BA, Stein DJ, Behm BW, Hays RA. Zinc Deficiency and the Recurrence of Clostridium difficile Infection after Fecal Microbiota Transplant: A Retrospective Cohort Study. J Nutr Metab. 2018 Oct 10;2018:9682975. doi: 10.1155/2018/9682975
Reed S, Neuman H, Moscovich S, Glahn RP, Koren O, Tako E. Chronic Zinc Deficiency Alters Chick Gut Microbiota Composition and Function. Nutrients. 2015 Nov 27;7(12):9768-84. doi: 10.3390/nu7125497.
Reed S, Neuman H, Moscovich S, Glahn RP, Koren O, Tako E. Chronic Zinc Deficiency Alters Chick Gut Microbiota Composition and Function. Nutrients. 2015 Nov 27;7(12):9768-84. doi: 10.3390/nu7125497.
Sauer AK, Grabrucker AM. Zinc Deficiency During Pregnancy Leads to Altered Microbiome and Elevated Inflammatory Markers in Mice. Front Neurosci. 2019 Nov 29;13:1295. doi: 10.3389/fnins.2019.01295.
Tian Y, Nichols RG, Cai J, Patterson AD, Cantorna MT4. Vitamin A deficiency in mice alters host and gut microbial metabolism leading to altered energy homeostasis. J Nutr Biochem. 2018 Apr;54:28-34. doi: 10.1016/j.jnutbio.2017.10.011.
Yang, J, Huang, K, Qin, S, Wu, X, Zhao, Z, Chen, F. Antibacterial Action of Selenium-Enriched Probiotics Against Pathogenic Escherichia coli. Dig Dis Sci. 2009 Feb;54(2):246-54. doi: 10.1007/s10620-008-0361-4.
Zackular JP, Moore JL, Jordan AT, Juttukonda LJ, Noto MJ, Nicholson MR, Crews JD, Semler MW, Zhang Y, Ware LB, Washington MK, Chazin WJ, Caprioli RM, Skaar EP. Dietary zinc alters the microbiota and decreases resistance to Clostridium difficile infection. Nat Med. 2016 Nov;22(11):1330-1334. doi: 10.1038/nm.4174.
Zackular JP, Skaar EP. The role of zinc and nutritional immunity in Clostridium difficile infection. Gut Microbes. 2018;9(5):469-476. doi: 10.1080/19490976.2018.1448354.
Zhang H, Liao X, Sparks JB, Luo XM. Dynamics of gut microbiota in autoimmune lupus. Appl Environ Microbiol. 2014 Dec;80(24):7551-60. doi: 10.1128/AEM.02676-14
The post 3 Food-Based Supplements for Your Gut Microbiome appeared first on The Paleo Mom.
!doctype>